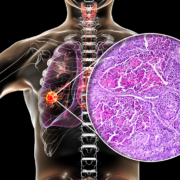
Biomarkers for improving lung cancer diagnosis, prognosis and treatment
Lung cancer has one of the lowest 5-year cancer survival rates as by the time a diagnosis is made, the disease has often reached the late stages. This article discusses how advances in understanding of the genetic evolution of cancer, the combi-nation of biomarker testing and CT scans can improve early diagnosis and touches on the use of biomarkers for improved patient selection for immune checkpoint inhibitor therapy.
by Managing Editor Alison Sleigh PhD
Background
In the UK, lung cancer is the second most common cancer in both men and women, accounting for 13.% of all new cancer cases in 2016 [1], and is the leading cause of death from cancer [2]. These statistics are also reflected in the United States of America [3]. In the UK, 5-year survival rates are low; on average, around 9.%. This is mainly because the majority of patients are already at late stage or metastatic disease at the point of diagnosis [1]. The main cause of lung cancer by far is smoking tobacco cigarettes. However, there are a number of other risk factors that should not be ignored. Environmental risk factors include exposure to radon, asbestos, pollution/poor air quality as well as infection. Genetics also plays a part because not all smokers develop lung cancer and a family history of the disease increases risk by around twofold [3]. In addition, genome-wide association studies have identified a number of chromosome regions that are associated with increased risk of lung cancer. Some of the first regions found have the strongest associations and include 5p15, 15q25-26 and 6p21. Mutations in the 15q25-26 region are linked to increased nicotine dependence and susceptibility for lung cancer. The 5p15 region contains the gene for telomerase reverse transcriptase, and mutations within this gene have been associated with adenocarcinomas in both smokers and non-smokers. Single nucleotide polymorphisms in the BAG6 gene on 6p21 are strongly associated with squamous cell carcinoma (see Bossé and Amos 2018 for a thorough review [4]). Interestingly, although smoking is the major primary cause of lung cancer, around 10–15.% of lung cancer patients have never smoked. Lung cancer in never smokers seems to occur most often in women and younger patients, involving
specific driver mutations such as in epidermal growth factor reductase (EGFR) gene and the echinoderm microtubule-associated protein-like 4 (EML4)–anaplastic lymphoma kinase (ALK) gene fusion, which gives rise to the ELM4-ALK fusion protein.
Diagnosis of lung cancer
Diagnosis of lung cancer usually occurs after a patient presents at a GP clinic with symptoms that can commonly include:
• a persistent cough
• coughing up blood
• persistent breathlessness
• unexplained tiredness and weight loss
• an ache or pain when breathing or coughing.
After this, diagnosis is confirmed by imaging (chest X-ray and then CT scan, and possibly also a PET-CT scan) and biopsy to confirm staging [5].
The challenges with diagnosis are that the early stages of the disease are symptomless; once symptoms become apparent, diagnosis often confirms late stage/metastatic disease, which has low survival rates. In addition, the methods of diagnosis are fairly invasive.
Screening programmes
Low-dose computed tomography (LDCT) screening of people with a higher risk of lung cancer has been trialled but has given with mixed results. Three smaller scale European trials showed non-significant effects or even an increase in mortality [6]. The largest trial, the National Lung Screening Trial, in the USA, showed much more promise with a 20.% reduction in lung cancer mortality [7]. However, the authors also reported an 18.% overdiagnosis rate: of the 24.2.% of patients classified as positive, 96.4.% were actually false positives. This means that 320 people need to be screened to prevent 1 lung cancer death, representing an unacceptable level of screening rounds, exposure to radiation, increased patient anxiety and costs.
Biomarkers
The use of biomarkers could, therefore, be a useful, non-invasive adjunct for identifying true/false positives from initial LDCT screening. Biomarkers can be non-invasively collected, and can come from the tumour itself, the tumour microenvironment as well as the host’s response to the tumour. Properly developed and validated, biomarkers can be diagnostic, prognostic and useful for monitoring therapy. There is, needless to say, a vast amount of research being done to discover such biomarkers for lung cancer and it is outwith the scope of this article to review it all. We will, however, discuss certain aspects of showing promise.
TRACERx: understanding the genetic development of lung cancer with circulating tumour DNA
TProfessor Charles Swanton at the Francis Crick Institute in London, UK, and his team have been analysing circulating tumour DNA (ctDNA) from individual non-small-cell lung cancer (NSCLC) patients through time, mapping the genetic evolution of the disease in a study known as TRACERx [Tracking NSCLC Evolution Through Therapy (Rx)]. In 2017, the initial results of 100 patients from a target group of 842 were published [8]. They found that although driver mutations in EGFR, MET, BRAF, and TP53 were almost always clonal, the heterogeneous driver alterations that occurred later in evolution (found in more than 75.% of the tumours) were common in PIK3CA and NF1 and in genes involved in chromatin modification and DNA damage response and repair. They also found that chromosomal instability was associated with intratumour heterogeneity and that elevated copy-number heterogeneity was associated with a significant increase in risk of recurrence or death [8]. Results from a more recent paper from the same consortium suggest that the immune microenvironment exerts a strong selection pressure in early-stage, untreated NSCLCs that produces multiple routes to immune evasion, which indicates a poor prognosis [9].
Early detection of Cancer of the Lung Scotland: diagnosing lung cancer at an earlier stage with a tumour-associated autoantibodies
The Early detection of Cancer of the Lung Scotland (ECLS) study has just this month made public the results of their randomized controlled trial of Oncimmune’s EarlyCDT®–Lung test on over 12.000 volunteers in Scotland (NHS areas of Tayside, Greater Glasgow and Clyde, and Lanarkshire) [10]. The EarlyCDT®–Lung test is a commercially available ELISA-based blood test that measures a panel of seven tumour-associated autoantibodies: p53, NY-ESO-1, CAGE, GBU4–5, SOX2, HuD and MAGE A4. The volunteers were asymptomatic adults aged between 50 amd 75 who had a high risk of developing lung cancer over the next 24 months. Participants who tested positive were followed up with chest X-ray and non-contrast CT scan. During the study period 127 participants were diagnosed with lung cancer; 41.% of patients from the intervention group who went on to develop cancer were diagnosed with early-stage cancer compared with only 26.8.% from the control group. The results showed that using a combination of the blood test with CT imaging gave a significant decrease in the late-stage diagnosis of lung cancer. The patients will now be followed over the next 5 years to determine mortality outcomes.
Immune checkpoint inhibitor therapy: biomarkers for better patient selection
In recent years, immune checkpoint inhibitor (ICI) therapy has been revolutionizing cancer treatment. This ‘cancer immunotherapy’ uses monoclonal antibodies that typically target programmed death 1 (PD-1), programmed death-ligand 1 (PD-L1), or cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), allowing the restoration of the cytotoxic immune response. However, while some patients respond very well to ICIs, many do not and even go on to develop hyper-progressive disease or immune-related adverse events. Hence, there is a need for biomarkers to aid the selection of patients who will benefit from this treatment. The recent review by Costantini et al. [11] discusses progress that is being made with a variety of types of biomarkers for this purpose, including soluble PD-L1, other soluble proteins (granzyme B, PD-L2, interleukine 2, interferon-gamma), ctDNA, the tumour mutational burden as well as effects of the gut microbiome.
Future perspectives
The work discussed here suggests that very positive steps can be taken towards reducing the mortality rate from lung cancer – probably not from any one aspect alone, but by using many approaches in combination: better biomarker testing will allow an initial screening and improvements in the analysis of CT scans (such as by artificial intelligence [12]) will both help to reduce rates of false positives and minimize the need for unnecessary invasive biopsies. These kinds of improvements may help to generate more cost-effective screening therefore encourage increased role out of lung cancer screening programmes. The rise in popularity of electronic nicotine delivery systems (vaping), particularly in the under 35s, is often thought of as a ‘safe’ way to smoke. However, there have now been 450 cases of a vaping-linked lung illness in the USA, perhaps heralding a need for a different sort of biomarker.
References
1. Lung cancer statistics. Cancer Research UK
(https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/lung-cancer)
2. Smittenaar CR, Petersen KA, Stewart K, Moitt N. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer 2016; 115(9): 1147–1155.
3. de Groot PM, Wu CC, Carter BW, Munden RF.
The epidemiology of lung cancer. Transl Lung Cancer Res. 2018; 7(3): 220–233.
4. Bossé Y, Amos C. A decade of GWAS results in lung cancer. Cancer Epidemiol Biomarkers Prev 2018; 27(4): 363–379.
5. Lung cancer: diagnosis. NHS website 2019.
(https://www.nhs.uk/conditions/lung-cancer/diagnosis/).
6. Sozzi G, Boeri M. Potential biomarkers for lung cancer screening. Transl Lung Cancer Res 2014; 3(3): 139–148.
7. National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, et al. Reduced lung cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365(5): 395–409.
8. Jamal-Hanjani M, Wilson GA, McGranahan N, Birkbak NJ, Watkins TBK, Veeriah S, Shafi S, Johnson DH, Mitter R, et al. Tracking the evolution of non-small cell lung cancer.
N Engl J Med 2017; 376(22): 2109–2121.
9. Rosenthal R, Cadieux EL, Salgado R, Bakir MA, Moore DA, Hiley CT, Lund T, Tanić M, Reading JL, et al. Neoantigen-directed immune escape in lung cancer evolution. Nature 2019; 567(7749): 479–485.
10. Sullivan F. PL02.03 – Early Detection of Cancer of the Lung Scotland (ECLS): trial results. Presented at the 2019 World Conference on Lung Cancer, Barcelona, Spain (https://library.iaslc.org/conference-program?product_id=15&author=&category=&date=2019-09-09&session_type=Plenary%20Session&session=&presentation=&keyword=sullivan&cme=undefined&).
11. Costantini A, Takam Kamga P, Dumenil C, Chinet T, Emile JF, Giroux Leprieur E. Plasma biomarkers and immune checkpoint inhibitors in non-small cell lung cancer: new tools for better patient selection? Cancers (Basel) 2019; 11(9): pii: E1269.
12. Ardila D, Kiraly AP, Bharadwaj S, Choi B, Reicher JJ, Peng L, Tse D, Etemadi M, Ye W, et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat Med 2019; 25(6): 954–961.