Biomarkers for improving the diagnosis of acute interstitial nephritis
Acute interstitial nephritis (AIN) may be the cause of more than 15 % of instances of acute loss of kidney function. Diagnosed early, it can often be successfully treated; however, lack of obvious symptoms means it can be easily missed. Left untreated, AIN can progress to chronic kidney disease. Currently, clinical diagnosis is confirmed by invasive biopsy. The development of noninvasive biomarkers is needed for improving early AIN diagnosis and therapeutic outcomes.
Background
Acute interstitial nephritis (AIN) is the inflammation of the kidney interstitium, an area surrounding the renal tubules consisting of fluid and extracellular matrix cells [1]. AIN is generally uncommon (<1 % incidence) in people with no symptoms but is thought to be the cause of more than 15 % of instances of acute loss of kidney function [2, 3].
Causes and symptoms
AIN can be caused by a variety of factors including environmental factors, infection and systemic disease. However, it is most usually seen as a result of adverse reaction to certain medications, such as antibiotics, antivirals, analgesics, gastrointestinal medications, antiseizure medication, diuretics and chemotherapy. When first described, the classic triad of AIN symptoms involved rash, joint pain and eosinophilia, similar to that of an allergic reaction. Fever was also present in 30–50 % of patients. A number of general and vague symptoms, such as nausea, vomiting, fatigue and lack of appetite, were also associated. However, more recently, AIN is more often caused by modern drugs, such as proton pump inhibitors and immune checkpoint inhibitors used in chemotherapy [3] and symptoms, if present, can be very subtle.
Treatment and prognosis
AIN can be treated (unlike other causes of acute loss of kidney function) if detected early by removal of the cause – such as the medication or treatment of the infection. Early treatment results in complete regain of kidney function in approximately 65% of cases, partial resolution in around 20% and irreversible damage in the remainder [4]. Although definitions have been developed and adopted into routine use for acute kidney injury (AKI: abrupt decrease in kidney function occurring over 7 days or less) and chronic kidney disease (CKD: persistence of kidney disease for a period of more than 90 days), there is an increasing awareness that AKI and CKD are not necessarily separate but may represent different stages along a continuum. For patients who develop AKI but then have ongoing pathology, the term acute kidney disease (AKD) has been developed [5]. AIN is an example of this as delayed diagnosis of this condition is more likely to result in incomplete recovery of kidney function and progression to CKD. It has been estimated that 40–60 % of AIN cases progress to CKD and that 2–3 % of CKD cases could be from undiagnosed AIN caused by proton pump inhibitor use [6, 7].
Methods of diagnosis
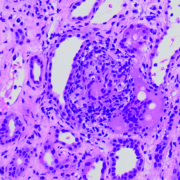
As we have seen, early diagnosis of AIN is crucial for the best prognosis; however, drug-induced AIN can develop over several days or weeks and the previously described ‘typical’ triad of symptoms is often absent. Physicians need to be aware of a range of more mild and varied symptoms such as flank pain, blood in the urine and joint pain. The main differential diagnosis is acute tubular necrosis (ATN) and the distinguishing features can be seen in Table 2 in Raghavan and Eknoyan’s 2014 paper [4]. Current laboratory tests include testing for markers of tubular dysfunction, which vary depending on the main site of injury; microscopic analysis of urine for the presence of protein, blood and eosinophils; and imaging studies. However, none of these tests are specific for AIN, with the only definitive diagnosis being given by kidney biopsy and even then histological examination needs to be performed by several pathologists.
Biomarkers for AIN
A number of biomarkers are available for the detection of AKI, such as monocyte chemotactic protein-1 (MCP-1), neutrophil gelatinase-associated lipocalin (NGAL), transforming growth factor beta 1 (TGF-β), etc; however, as mentioned by Raghavan and Eknoyan, these have been developed to diagnose AKI based on its definition of increased serum creatinine, which for AIN is too late for the best hope of regaining good kidney function [4 and references therein]. Recently, though, a new study by Moledina and colleagues has identified two new urine biomarkers that improve prebiopsy diagnosis of AIN [7]. The authors postulated that as AIN is caused by certain T-cell subsets, specific T-cell cytokine levels might serve as biomarkers to distinguish AIN from other causes of AKD. Of 218 participants in the study, who had all had kidney biopsy for the evaluation of AKD, 32 were confirmed with AIN and the remaining 186 who did not have AIN were used as controls. After testing 22 selected urine and plasma cytokines, they found two, tumour necrosis factor alpha (TNF-α) and interleukin (IL)-9, that were present at consistently higher levels in the urine of AIN patients and were diagnostic of AIN. The authors conclude “inclusion of urinary TNF-α and IL-9 improves discrimination over clinicians’ prebiopsy diagnosis and currently available tests for AIN diagnosis” [7]. In another recent paper from the same group, the authors demonstrate that the use of urinary TNF-α and IL-9 biomarkers also allows the differentiation of AIN over ATN [8].
Summary
Diagnosis of drug-induced AIN at a stage early enough to limit irreversible kidney damage is challenging because of a lack of conclusive symptoms and the gold standard diagnosis of kidney biopsy is invasive, not suitable for all patients and fraught with low inter-rater agreement. The results of the study by Moledina et al. demonstrate that testing for urine biomarkers TNF-α and IL-9 is a useful addition to a clinician’s prebiopsy diagnosis and might be able to eventually replace the need for kidney biopsy. The use of these biomarkers may be a welcome step for maximizing the chances of complete kidney function recovery and limiting the number of patients who progress to CKD.
References
1. Zeisberg M, Kalluri R. Physiology of the renal interstitium. Clin J Am Soc Nephrol 2015; 10(10): 1831–1840.
2. Brewster UC, Rastegar A. Acute Interstitial Nephritis. In: National Kidney Foundation’s primer on kidney diseases, eds Gilbert SJ, Weiner DE, Bomback AS, Parazella MA, Tonelli M, 7th edn; pp320–325. Elsevier 2017. ISBN 978-0323477949.
3. Mamlouk O, Selamet U, Machado S, Abdelrahim M, Glass WF, et al. Nephrotoxicity of immune checkpoint inhibitors beyond tubulointerstitial nephritis: single-center experience. J Immunother Cancer 2019; 7(1): 2.
4. Raghavan R, Eknoyan G. Acute interstitial nephritis – a reappraisal and update. Clin Nephrol 2014; 82(3): 149–62.
5. Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 2017; 13(4): 241–257.
6. Lazarus B, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med 2016; 176(2): 238–246.
7. Moledina DG, Wilson FP, Pober JS, Perazella MA, Singh N, et al. Urine TNF-α and IL-9 for clinical diagnosis of acute interstitial nephritis. JCI Insight 2019; 4(10): pii: 127456.
8. Moledina DG, Parikh CR. Differentiating acute interstitial nephritis from acute tubular injury: a challenge for clinicians. Nephron 2019; doi: 10.1159/000501207 [Epub ahead of print].