Biomarkers for the prediction of clinically significant prostate cancer
Prostate cancer is the most common cancer in men and diagnosis involves a combination of assessments. Levels of the biomarker prostate-specific antigen (PSA) are commonly measured, but do not always equate to cancer status. Testing of PSA in combination with other biomarkers may help to improve diagnostic and prognostic accuracy, as well as minimizing overdiagnosis as well as unnecessary intervention. This article provides a summary of the information currently known about biomarkers showing promise for use in prostate cancer screening.
by Dr Alexandra Tabakin, Dr Sung Un Bang and Dr Isaac Y. Kim
Introduction
Prostate cancer is the most commonly diagnosed cancer type in the USA and second leading cause of cancer deaths in men. In 2018, there will be an estimated 164 690 new cases with an estimated 29 430 deaths [1]. Although many prostate cancers are indolent in nature and can be safely monitored with active surveillance, a significant proportion of patients will require intervention with surgery, radiation, or other therapies. One of the major challenges in treating prostate cancer is risk stratification and differentiating clinically significant prostate cancers in order to avoid overdiagnosis and overtreatment [2]. To do so, patients undergo risk stratification, which conventionally includes a combination of prostate-specific antigen (PSA) screening, digital rectal exam (DRE), trans-rectal ultrasonography (TRUS)-guided biopsy. Currently clinically insignificant prostate cancer, according to Epstein criteria, is defined as cancer with preoperative PSA <10ng/ml, clinical stage <T1c, Gleason score <6, PSA density <0.15, <2 positive biopsy cores, and <50% cancer involvement in any core [3–5]. However, as we learn more about the heterogeneity of prostate cancer tumours, various serum biomarkers have been investigated to improve diagnostic and prognostic accuracy and minimize treatment. In this review, we discuss various biomarkers and their utilization for the prediction of clinically significant prostate cancer.
Serum biomarkers
PSA
PSA, or prostate-specific antigen, is a serine protease released by the prostate. PSA gained notoriety in the 1980s when it was reported to have various uses including screening, monitoring disease progression, and detecting recurrence of the cancer. As PSA screening for prostate cancer increased, the incidence of prostate cancer also rose in the 1990s. However, PSA only has a 25–40% specificity rate for prostate cancer and can be elevated with infection, trauma, and benign prostatic hyperplasia (BPH) [6]. In fact, about 15% of men with a low level of PSA (<4.0 ng/ml) have prostate cancer [7].
Because the harms of biopsy and prostate cancer treatment may outweigh the benefits in some patients with clinically insignificant prostate cancer, efforts have been made to improve the validity of PSA in differentiating benign conditions and prostate cancer. One such effort is the use of free PSA; those with an elevated PSA and a lower serum percentage of free PSA (%f-PSA) are more likely to have BPH rather than prostate cancer [8]. The Prostate Health Index (PHI) formula incorporates serum total PSA, free PSA, and the [−2]proPSA to discriminate Gleason 3+4 and greater cancers with 90% sensitivity and 17% specificity [9]. 4K score is another novel test which is comprised of total PSA, free PSA, intact PSA, and human kallikrein-related peptidase 2 to detect clinically significant prostate cancer and discern those who would benefit from a prostate biopsy while preventing 30–58% of biopsies [10].
PAP
Prostatic acid phosphatase (PAP) was the first popularized prostate cancer serum biomarker, but was eventually replaced by PSA, as it is less sensitive in diagnosing prostate cancer and detecting recurrence. Elevated PAP level has been associated with a high risk of bone metastases [11], significantly shortened overall survival [12] as well as disease-free survival [13], and increased risk of biochemical recurrence [14]. Interestingly, recent studies have shown that PAP may be useful in detecting high-risk clinically significant prostate cancer patients; it is speculated that PAP may be associated with micro-metastatic disease prior to treatment, and therefore, predict response to treatment [15].
NLR, ANC, ALC
Inflammation and tissue microenvironment are important factors in cancer development. Although the temporal relationship is not well established, a lymphocyte-mediated immune response is thought to occur early in the development of prostate cancer. Neutrophil-to-lymphocyte ratio (NLR) compares the activity of both neutrophils and lymphocytes in the inflammatory response. NLR is a useful prognostic biomarker in mCRPC, where a higher score correlates less relative lymphocyte activity and a worse prognosis. When looking at localized low-risk prostate cancer, studies have shown that NLR is not associated with upstaging, upgrading, or biochemical recurrence. However, increased absolute lymphocyte count (ALC) and absolute neutrophil count (ANC) were associated with upstaging and lower 5-year biochemical recurrence-free survival. More development on these markers may guide clinicians in re-stratifying patients who meet conventional criteria for low-risk prostate cancer [16].
Urine biomarkers
PCA3
Urinary prostate cancer antigen 3 (PCA3) is among the most promising non-invasive biomarker among non-PSA based tests, as it is overexpressed in over 95% of prostate cancers [6]. PCA3 is a long noncoding RNA collected from shed prostate cells during urination. PCA3 is a more specific biomarker for prostate cancer because, unlike PSA, PCA3 levels are not influenced by prostate size, BPH, prostatitis, or the use of 5α-reductase inhibitors [17]. At the genetic level, PCA3 may help distinguish between prostate cancer and high-grade prostatic intraepithelial neoplasia (HG-PIN), as PCA3 is seldom expressed in HG-PIN [18]. Several studies have demonstrated that a higher PCA3 score correlates with clinically significant prostate cancer and larger tumour volume, therefore potentially aiding in selecting patients for active surveillance [19]. In 2012, the FDA approved the PROGENSA PCA3 assay predict men who would benefit from a repeat biopsy in those with a previous negative prostate biopsy [6]. In a recent meta-analysis of 46 clinical trials, the sensitivity and specificity of PROGENSA PCA3 was 65% and 73%, respectively [20].
Genetic mutations
TMPRSS2::ERG
TMPRSS2::ERG, or T2:ERG, gene fusions constitute 90% of gene fusions implicated in prostate cancer, as well as half of all prostate cancers [21, 22]. When the androgen responsive regulatory element TMPRSS2 and the gene for the transcription factor ERG are fused together, androgen-driven genes are overexpressed and tumorigenesis occurs [21]. When used alone, urinary T2:ERG RNA has a reported 86% specificity and 45% sensitivity in prostate cancer detection. However, when used in conjunction with PCA3, specificity and sensitivity improve to 90% and 80%, respectively [6, 23]. Moreover, this test may prevent up to 42% of unnecessary biopsies, limiting healthcare costs [24].
PTEN
Loss of the tumour-suppressor gene, PTEN, or phosphatase and tensin homologue, leading to activation of the PI3K/AKT/mTOR signalling has been found in both early stage and castrate-resistant prostate cancers. Preclinical data show that PI3K pathway activation is related to resistance to androgen deprivation, leading to disease progression and poor response to treatment. In mouse models, conditional deletion of PTEN initially led to the development of prostate hyperplasia and later on invasive and metastatic prostate cancers likely by modulating the p110β catalytic subunit of PI3K. In addition, ablation of p110β hindered AKT signalling and reduced tumorigenesis [25]. In a cohort of 77 men, loss of PTEN at initial prostate biopsy was predictive of the development of castrate-resistant prostate cancer, response to androgen deprivation therapy, and prostate-cancer-specific mortality [26]. Additionally, decreased PTEN expression has been associated with increased risk of biochemical and clinical recurrence after prostatectomy [27]. Therefore, the association between castrate-resistant prostate cancer and PTEN loss as well as PI3K/AKT/mTOR pathway activation suggests that PTEN may have prognostic value in prostate cancer risk stratification.
CHD1
The CHD1 gene, encoding chromodomain helicase DNA-binding protein 1, is commonly deleted in 10–26% of all prostate cancers. The loss of CHD1 affects the ability to repair DNA double-strand breaks via homologous recombination. CHD1 deletion has generally been associated with a poor prognosis. However, studies have demonstrated tumours with CHD1 deletions to be sensitive to both PARP inhibitors and carboplatin, both in vitro and in vivo, suggesting that future research may be able to identify to response to treatment based off of tumour genotypes [28].
Circulating biologics
Circulating tumour cells
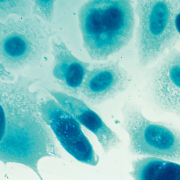
Circulating tumour cells (CTCs) are defined as cells that leave the site of a primary cancer, travel through the bloodstream, and settle at other sites in the body where they grow into new tumours, or metastases [29]. In 2004, CellSearch Circulating Tumor Cell System was approved by the FDA as an assay for enumerating CTCs. In recent studies, CTC count, deemed the ‘liquid biopsy’, has been shown to have a role in predicting overall survival and response to treatment, risk stratification, and detecting metastases. In addition, using CTCs to detect biomarkers, such as ERG, PTEN, and AR may allow for personalized treatments based on tumour genomes [9, 30].
Circulating exosomes
Circulating prostate cancer-related exosomes are double-membrane vesicles carrying RNA and pro-oncogenic molecules, which induce malignant transformation in normal cells. ExoDx prostate Intelliscore urine exosome assay (developed by Exosome Diagnostics Inc.) detects exosomal RNA expression of ERG, PCA3 and SPDEF (SAM pointed domain containing ETS transcription factor) in voided urine samples. A score is generated that is able to predict high-grade prostate cancer (Gleason >7) with a negative predictive value of 91%. This assay may be useful in discriminating clinically significant prostate cancer and reducing the number of unnecessary biopsies [31].
Conclusion
The emergence and widespread usage of PSA as a routine screening test for prostate cancer allows for early detection and risk stratification. Testing for PSA in combination with novel biomarkers such as PCA3, TMPRSS2::ERG, PTEN, and others may improve our diagnostic abilities, given the heterogeneity of prostate cancers and their treatments. There are many challenges in establishing useful biomarkers including creating affordable and accessible testing, determining cut-offs, and determining accuracy. As the clinical utility of these biomarkers is further defined, we hope to better risk stratify patients and select appropriate treatments early on in diagnosis. Further research efforts should focus on the synergism between the Epstein criteria, biomarker utility, and how to best bring these tools from bench to bedside.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68(1): 7–30.
2. Lees K, Durve M, Parker C. Active surveillance in prostate cancer: patient selection and triggers for intervention. Curr Opin Urol 2012; 22(3): 210–215.
3. D’Amico AV, Whittington R, Malkowicz SB, Weinstein M, Tomaszewski JE, Schultz D, et al. Predicting prostate specific antigen outcome preoperatively in the prostate specific antigen era. J Urol 2001; 166(6): 2185–2188.
4. Epstein JI, Chan DW, Sokoll LJ, Walsh PC, Cox JL, Rittenhouse H, et al. Nonpalpable stage T1c prostate cancer: prediction of insignificant disease using free/total prostate specific antigen levels and needle biopsy findings. J Urol 1998; 160(6): 2407–2411.
5. Klotz L, Zhang L, Lam A, Nam R, Mamedov A, Loblaw A. Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol 2010; 28(1): 126–131.
6. Sanguedolce F, Cormio A, Brunelli M, D’Amuri A, Carrieri G, Bufo P, et al. Urine TMPRSS2: ERG fusion transcript as a biomarker for prostate cancer: literature review. Clin Genitourin Cancer 2016; 14(2): 117–121.
7. Prensner JR, Rubin MA, Wei JT, Chinnaiyan AM. Beyond PSA: the next generation of prostate cancer biomarkers. Sci Transl Med 2012; 4(127): 127rv3.
8. Grossklaus DJ, Smith JA, Shappell SB, Coffey CS, Chang SS, Cookson MS. The free/total prostate-specific antigen ratio (%fPSA) is the best predictor of tumor involvement in the radical prostatectomy specimen among men with an elevated PSA. Urol Oncol 2002; 7(5): 195–198.
9. Chistiakov DA, Myasoedova VA, Grechko AV, Melnichenko AA, Orekhov AN. New biomarkers for diagnosis and prognosis of localized prostate cancer. Semin Cancer Biol 2018; doi: 10.1016/j.semcancer.2018.01.012.
10. Parekh DJ, Punnen S, Sjoberg DD, Asroff SW, Bailen JL, Cochran JS, et al. A Multi-institutional prospective trial in the USA confirms that the 4Kscore accurately identifies men with high-grade prostate cancer. Eur Urol 2015; 68(3): 464–470.
11. Whitesel JA, Donohue RE, Mani JH, Mohr S, Scanavino DJ, Augspurger RR, et al. Acid phosphatase: its influence on the management of carcinoma of the prostate. J Urol 1984; 131(1): 70–71.
12. Johnson DE, Prout GR, Scott WW, Schmidt JD, Gibbons RP, et al. Clinical significance of serum acid phosphatase levels in advanced prostatic carcinoma. Urology 1976; 8(2): 123–126.
13. Moul JW, Connelly RR, Perahia B, McLeod DG. The contemporary value of pretreatment prostatic acid phosphatase to predict pathological stage and recurrence in radical prostatectomy cases. J Urol 1998; 159(3): 935–940.
14. Han M, Piantadosi S, Zahurak ML, Sokoll LJ, Chan DW, Epstein JI, et al. Serum acid phosphatase level and biochemical recurrence following radical prostatectomy for men with clinically localized prostate cancer. Urology 2001; 57(4): 707–711.
15. Faiena I, Kim S, Farber N, Kwon YS, Shinder B, Patel N, et al. Predicting clinically significant prostate cancer based on pre-operative patient profile and serum biomarkers. Oncotarget 2017; 8(65): 109783–109790.
16. Kwon YS, Han CS, Yu JW, Kim S, Modi P, Davis R, et al. Neutrophil and lymphocyte counts as clinical markers for stratifying low-risk prostate cancer. Clin Genitourin Cancer 2016; 14(1): e1–8.
17. Roobol MJ, Schröder FH, van Leeuwen P, Wolters T, van den Bergh RCN, van Leenders GJLH, et al. Performance of the prostate cancer antigen 3 (PCA3) gene and prostate-specific antigen in prescreened men: exploring the value of PCA3 for a first-line diagnostic test. Eur Urol 2010; 58(4): 475–481.
18. Wei W, Leng J, Shao H, Wang W. High PCA3 scores in urine correlate with poor-prognosis factors in prostate cancer patients. Int J Clin Exp Med 2015; 8(9): 16606–16612.
19. Ploussard G, Epstein JI, Montironi R, Carroll PR, Wirth M, Grimm M-O, et al. The contemporary concept of significant versus insignificant prostate cancer. Eur Urol 2011; 60(2): 291–303.
20. Cui Y, Cao W, Li Q, Shen H, Liu C, Deng J, et al. Evaluation of prostate cancer antigen 3 for detecting prostate cancer: a systematic review and meta-analysis. Sci Rep 2016; 6: 25776.
21. Burkhardt L, Fuchs S, Krohn A, Masser S, Mader M, Kluth M, et al. CHD1 is a 5q21 tumor suppressor required for ERG rearrangement in prostate cancer. Cancer Res 2013; 73(9): 2795–2805.
22. Tomlins SA, Laxman B, Varambally S, Cao X, Yu J, Helgeson BE, et al. Role of the TMPRSS2-ERG gene fusion in prostate cancer. Neoplasia 2008; 10(2): 177–188.
23. Salami SS, Schmidt F, Laxman B, Regan MM, Rickman DS, Scherr D, et al. Combining urinary detection of TMPRSS2: ERG and PCA3 with serum PSA to predict diagnosis of prostate cancer. Urol Oncol 31(5): 566–571.
24. Sanda MG, Feng Z, Howard DH, Tomlins SA, Sokoll LJ, Chan DW, et al. Association between combined TMPRSS2:ERG and PCA3 RNA urinary testing and detection of aggressive prostate cancer. JAMA Oncol 2017; 3(8): 1085–1093.
25. Crumbaker M, Khoja L, Joshua AM. AR Signaling and the PI3K pathway in prostate cancer. Cancers 2017; 9(4): doi: 10.3390/cancers9040034.
26. Mithal P, Allott E, Gerber L, Reid J, Welbourn W, Tikishvili E, et al. PTEN loss in biopsy tissue predicts poor clinical outcomes in prostate cancer. Int J Urol 2014; 21(12): 1209–1214.
27. Chaux A, Peskoe SB, Gonzalez-Roibon N, Schultz L, Albadine R, Hicks J, et al. Loss of PTEN expression is associated with increased risk of recurrence after prostatectomy for clinically localized prostate cancer. Mod Pathol 2012; 25(11): 1543–1549.
28. Kari V, Mansour WY, Raul SK, Baumgart SJ, Mund A, Grade M, et al. Loss of CHD1 causes DNA repair defects and enhances prostate cancer therapeutic responsiveness. EMBO Rep 2016; 17(11): 1609–1623.
29. West H, Jin JO. Circulating tumor cells. JAMA Oncol 2015; 1(3): 394.
30. Galletti G, Portella L, Tagawa ST, Kirby BJ, Giannakakou P, Nanus DM. Circulating tumor cells in prostate cancer diagnosis and monitoring: an appraisal of clinical potential. Mol Diagn Ther 2014; 18(4): 389–402.
31. McKiernan J, Donovan MJ, O’Neill V, Bentink S, Noerholm M, Belzer S, et al. A novel urine exosome gene expression assay to predict high-grade prostate cancer at initial biopsy. JAMA Oncol 2016; 2(7): 882–889.
The authors
Alexandra Tabakin MD,
Sung Un Bang MD, Isaac Yi Kim MD PhD
Section of Urologic Oncology, Rutgers Cancer Institute of New Jersey and Division of Urology, Rutgers Robert Wood Johnson Medical School, Rutgers, The State University of New Jersey, New Brunswick, NJ, USA
*Corresponding author
E-mail: kimiy@cinj.rutgers.edu