Therapeutic drug monitoring of antiepileptic drugs
Antiepileptic drugs (AEDs) are widely used and their number is steadily increasing. Therapeutic drug monitoring of AEDs, when performed correctly, can be a valuable tool for the treating physician. This article describes the indications, limitations and pitfalls that must be observed when measuring and interpreting AED serum concentrations.
by Dr Arne Reimers and Prof. Eylert Brodtkorb
Why measure antiepileptic drug serum concentrations?
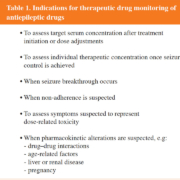
Antiepileptic drugs (AEDs) are widely used, not only for epilepsy, but also for a range of non-epilepsy conditions, such as bipolar (manic-depressive) disorder, migraine and neuropathic pain [1]. Thus, the total number of AED users substantially exceeds the number of people with epilepsy. Therapeutic drug monitoring (TDM) has for many years been used to support AED treatment, as many of these drugs have unfavourable pharmacokinetic properties, a potential to problematic drug interactions as well as narrow therapeutic windows. TDM is a means of assisting clinical decision-making and should always be done with a specific question in mind. The general indications for TDM of AEDs are listed in Table 1.
Non-linear and linear pharmacokinetics
TDM of AEDs has a long clinical tradition. When the concept of TDM was introduced in the early 1970s, phenytoin was one of the first drugs to which it was applied [2]. This was mainly because phenytoin, then one of the most frequently used AEDs, has so-called non-linear pharmacokinetics. Linear kinetics means that the serum concentration is linearly correlated with dose – a doubling of the dose will double the serum concentration. This applies to almost all medicinal drugs. However, some drugs exhibit non-linear or saturation kinetics; phenytoin is one of them. Doubling the phenytoin dose may result in an unpredictable increase of the serum concentration. Thus, monitoring the phenytoin serum concentration was desirable and soon became available in large parts of the world.
Most other AEDs, however, exhibit linear kinetics. Why then is it important to measure their serum concentrations? One reason is the nature of epilepsy itself and the issue of prophylactic treatment. The only clinical marker for successful management is the extent of seizure control. However, epileptic seizures may occur in random patterns. The intervals between seizures may be minutes or months, and if a seizure occurs, it may have dramatic consequences, not only for the patient, but even for others. Thus, it can be very demanding to evaluate the therapeutic effect of AED treatment by clinical observation alone.
Absorption, distribution, metabolism and excretion
In addition, the pharmacokinetics of AEDs may be affected by changes in absorption, distribution, metabolism and excretion (ADME). Co-morbidity, pregnancy, drug interactions, pharmacogenetic polymorphisms, etc, all may considerably affect the ADME of AEDs (Fig. 1). Pregnancy may induce pronounced pharmacokinetic alterations, including increased volume of distribution, elevated renal clearance, and induction of hepatic metabolism. Breakthrough seizures in previously seizure-free patients may occur [3–5].
The serum concentration of carbamazepine may rise threefold and produce toxic symptoms when the patient is prescribed certain antibiotics which inhibit its metabolism, such as erythromycin. On the other hand, carbamazepine and other inducers of hepatic metabolism, may reduce serum concentrations of several other drugs, among them valproate, lamotrigine and hormonal contraceptives. Valproate is also a potent inhibitor of drug-metabolizing liver enzymes and may double lamotrigine concentrations. The clinically important induction of the metabolism of lamotrigine by combined oral contraceptives was detected by routine use of TDM [6]. Gabapentin is excreted almost exclusively by the kidneys; hence reduced kidney function will give increased serum concentrations.
Adherence
Poor adherence to prescribed treatment is one of the most important obstacles to the management of epilepsy [7, 8]. It has been documented that roughly half of all patients take their medicine more or less irregularly [9]. A recent study in patients admitted to hospital with acute epileptic seizures found that almost 40 % had less than 75 % of their usual trough AED serum concentration, indicating one or more missed doses [8] (Fig. 2). In such situations, it is crucial that the treating clinician receives the lab result as soon as possible to be able to decide on how to proceed with the management of the patient. Should the daily AED dose be increased or not? In the event that the seizure occurred because of a missed intake, it would not be appropriate; dose increase could even be harmful to the patient. If the serum concentration was adequate (according to prescribed dose), the occurrence of a seizure would suggest that the daily dose was too low and should be increased. This decision must be made quickly as the patient usually will be dismissed from hospital the next morning. It is essential to identify pseudo-refractory epilepsy. Clinically unrecognized non-adherence is often mistaken as drug-resistant epilepsy [10].
How it is normally done
The common convention is that blood samples for measuring the concentration of AEDs be taken drug-fasting in the morning (i.e. from 12 h to a maximum of 24 h after the last dose intake, and before the morning dose). Also, the patient must be in pharmacological steady state. This means that the amount of drug administered per unit time is in equilibrium with the amount of drug eliminated from the body during the same time. For all drugs, this state is reached after five times the drug’s plasma half-life. These rules apply after every dose change (Fig. 2E). The difficulties in complying with these rules are an important obstacle to TDM and is one major reason its routine use is discredited in many parts of the world. If a blood sample is taken before steady state is reached, or when the patient is not drug-fasting, the interpretation of the measured blood concentration is tricky and requires profound clinical-pharmacological experience.
Most commonly, the analyses are performed in a central lab using serum or plasma, either with immunologic or chromatographic methods. Usually, the total AED concentration (protein-bound plus unbound drug) is measured. In certain situations, e.g. in the elderly with hypoalbuminemia or in pregnant women, it is desirable to measure the unbound (free) proportion of an AED. This applies mainly to valproate and phenytoin which are >90 % protein bound. Hypoalbuminemia may cause signs of overdose despite only modest total AED concentration. However, unbound concentrations are rarely requested and not offered by all labs.
Reference ranges for antiepileptic drugs
It must be noted that reference ranges (RRs) for AEDs apply to the treatment of epilepsy. RRs for bipolar disorder have been suggested [11] but are not broadly established, whereas in the treatment of chronic pain states, treatment is usually guided by the clinical response alone. Unfortunately, with few exceptions, most RRs are not well documented. The exceptions are those AEDs that have been around for decades, e.g. phenytoin, carbamazepine and valproate. For them, broadly accepted RRs are supported by long clinical experience.
For the newer AEDs (introduced after 1990), there is a considerable lack of data. One of the reasons for the poor documentation is that drug manufacturers rarely publish serum concentrations obtained in clinical phase III or IV studies. Another reason is a lack of studies specifically aimed at examining the correlation between serum concentrations and effect. Thus, RRs for AEDs are often based on extrapolation of pharmacokinetic data obtained in preclinical studies, or on data from large routine databases, i.e. by applying some sort of population kinetics. Such data often lack clinical correlates owing to incomplete information provided on the request forms.
One consequence of the above is that the RRs used by different labs, and reported in the literature, are often incoherent. Another weakness of these population-based RRs is the fact that many patients achieve a satisfactory therapeutic effect with serum concentrations below the RR, while others need concentrations above the RR, yet without suffering symptoms of overdose. This is also the reason why the term ‘therapeutic range’ should not be used; it wrongly implies that any concentration outside that range is ‘non-therapeutic’.
The concept of individual RRs where each patient serves as his/her own reference [12] is an alternative approach. An obvious prerequisite for this concept is the availability of several consecutive serum concentration measurements (within reasonable time intervals) in the individual patient as well as close clinical follow-up, to correlate various serum concentrations with their corresponding clinical effect. It would also be desirable to have non-sufficient concentrations as well as toxic concentrations. Most of these individual therapeutic ranges would fall within the population-derived RRs. However, as mentioned above, some patients respond well to concentrations outside the common RR. For the sake of clarity, it has been suggested that such individual RRs be called individual therapeutic ranges [13]. Despite its advantages, neither the concept itself nor the term individual therapeutic range can be regarded as generally established.
Concluding remarks
TDM of AEDs is controversial, as it has been repeatedly emphasized that ‘treating patients is more important than treating blood levels’ [14]. Clinical evaluation and follow-up will continue to be the leading element in the management of epilepsy.
Nevertheless, when correctly applied, appropriately sampled and analysed, as well as correctly interpreted, TDM stands out as an important and relatively inexpensive tool for optimizing the drug treatment of epilepsy. Obviously, blinding for the actual serum concentrations may have severe untoward consequences in specific patient populations, such as pregnant women and patients with poor medication-taking behaviour.
References
1. Johannessen Landmark C. Antiepileptic drugs in non-epilepsy disorders: relations between mechanisms of action and clinical efficacy. CNS Drugs 2008; 22(1): 27–47.
2. Richens A. Drug estimation in the treatment of epilepsy. Proc R Soc Med 1974; 67(12 Pt 1): 1227–1229.
3. Cappellari AM, Cattaneo D, Clementi E, Kustermann A. Increased levetiracetam clearance and breakthrough seizure in a pregnant patient successfully handled by intensive therapeutic drug monitoring. Ther Drug Monit 2015; 37(3): 285–287.
4. Reimers A, Helde G, Becser Andersen N, Aurlien D, Surlien Navjord E, Haggag K, Christensen J, Lillestølen KM, Nakken KO, Brodtkorb E. Zonisamide serum concentrations during pregnancy. Epilepsy Res 2018; 144: 25–29.
5. Voinescu PE, Park S, Chen LQ, Stowe ZN, Newport DJ, Ritchie JC, Pennell PB. Antiepileptic drug clearances during pregnancy and clinical implications for women with epilepsy. Neurology 2018; 91(13): e1228–1236.
6. Sabers A, Buchholt JM, Uldall P, Hansen EL. Lamotrigine plasma levels reduced by oral contraceptives. Epilepsy Res 2001; 47(1–2): 151–154.
7. Faught E. Adherence to antiepilepsy drug therapy. Epilepsy Behav 2012; 25(3): 297–302.
8. Samsonsen C, Reimers A, Bråthen G, Helde G, Brodtkorb E. Nonadherence to treatment causing acute hospitalizations in people with epilepsy: an observational, prospective study. Epilepsia 2014; 55(11): e125–128.
9. Adherence to long-term therapies: evidence for action World Health Organization 2003; http://www.who.int/chp/knowledge/publications/adherence_report/en/.
10. Brodtkorb E, Samsonsen C, Sund JK, Bråthen G, Helde G, Reimers A. Treatment non-adherence in pseudo-refractory epilepsy. Epilepsy Res 2016; 122: 1–6.
11. Hiemke C, Bergemann N, Clement HW, Conca A, Deckert J, Domschke K, Eckermann G, Egberts K, Gerlach M, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry 2018; 51(1–02): 9–62.
12. Landmark CJ, Johannessen SI, Tomson T. Dosing strategies for antiepileptic drugs: from a standard dose for all to individualised treatment by implementation of therapeutic drug monitoring. Epileptic Disord 2016; 18(4): 367–83.
13. Patsalos PN, Berry DJ, Bourgeois BF, Cloyd JC, Glauser TA, Johannessen SI, Leppik IE, Tomson T, Perucca E. Antiepileptic drugs – best practice guidelines for therapeutic drug monitoring: a position paper by the subcommission on therapeutic drug monitoring, ILAE Commission on Therapeutic Strategies. Epilepsia 2008; 49(7): 1239–1276.
14. Chadwick DW. Overuse of monitoring of blood concentrations of antiepileptic drugs. Br Med J (Clin Res Ed) 1987; 294(6574): 723–724.
The authors
Arne Reimers*1,2 MD PhD and Eylert Brodtkorb3,4 MD PhD
1Dept. of Clinical Chemistry and Pharmacology, Division of Laboratory Medicine, Skåne University Hospital, Lund, Sweden
2Department of Clinical Chemistry and Pharmacology, Lund University, Lund, Sweden
3Dept. of Neuromedicine and Movement Science, Norwegian University of Science and Technology (NTNU), Trondheim, Norway
4Dept. of Neurology and Clinical Neurophysiology, St. Olavs University Hospital, Trondheim, Norway
*Corresponding author
E-mail: arne.reimers@med.lu.se