Use of immunohistochemistry in the determination of mismatch repair status of colorectal carcinoma
by Dr Odharnaith O’Brien, Dr Éanna Ryan and Prof. Kieran Sheahan
Introduction
Owing to recent remarkable advances in our understanding of the molecular and genetic basis of disease, it is now known that colorectal carcinoma (CRC) is a heterogenous clinical entity characterized by multiple molecular subtypes [1]. One such molecular pathway involved in CRC pathogenesis is the microsatellite instability (MSI) pathway, where a deficient mismatch repair (dMMR) system leads to unchecked errors in DNA replication [2]. These errors result in a propensity for abnormal insertion or deletion of short, repetitive sequences of DNA (microsatellites), resulting in mutations in cancer-related genes and ultimately neoplasia. Up to 15–20% of colorectal carcinomas are of MSI phenotype. An inherited predisposition to dMMR cancers, particularly CRC, is present in Lynch syndrome, the most common heritable cancer syndrome. It is due to autosomal dominant mutations in four mismatch repair (MMR) genes (MLH1, MSH2, MSH6, PMS2) or more rarely by mutations in EPCAM, a gene upstream of MSH2. Patients present at an earlier age and have an increased incidence of synchronous and metachronous CRCs. Histologically, tumours are poorly differentiated, frequently exhibiting a mucinous or signet ring cell morphology. Tumour infiltrating lymphocytes are often prominent and a Crohn’s-like inflammatory response may be present at the tumour periphery. However, the majority of dMMR CRCs arise sporadically and are a result of MLH1 promoter hypermethylation. Unlike in Lynch syndrome, these tumours affect the right side of the colon, are diagnosed at advanced age and have a female preponderance. They are, however, histologically similar to Lynch syndrome CRCs. Mutation of the BRAF V600E gene is present in 60–70% of sporadic dMMR tumours and is almost never seen in Lynch syndrome. As such, incorporating BRAF and/or MLH1 methylation status into MMR diagnostic algorithms offers potential exclusion criteria for genetic testing [3–5].
Why is it important to identify dMMR in colorectal carcinoma?
Diagnosing a patient with a dMMR cancer has a number of advantages:
1. Identification of patients with Lynch syndrome
Once diagnosed, these patients benefit from increased surveillance, prophylactic aspirin therapy and more radical surgery in order to facilitate the prevention and/or early detection of potential tumours (both colonic and extracolonic) [5].
2. It provides prognostic information
Several studies have shown that dMMR CRC has a better prognosis than MMR proficient (pMMR) CRC. dMMR tumours are less likely to develop lymph node and liver metastases. However, in advanced disease (stage IV) dMMR status can portend a poorer prognosis [6–8].
3. It provides predictive information
dMMR tumours likely have a reduced response to 5-flurouracil based chemotherapy. In addition, advanced dMMR tumours have been shown to have a better response rate and progression free survival to the anti PD-1 drug pembrolizumab when compared to pMMR tumours [7–9].
Reliance by clinicians on clinical criteria such as the revised Bethesda guidelines to determine which patients should undergo screening for Lynch syndrome results in inaccurate determination of eligibility for screening in up to 28% of cases [10]. Consequently, a number of organizations have recently published guidelines endorsing reflex MMR testing of all diagnosed CRCs, including the National Institute for Health and Care Excellence (NICE), the American Society for Clinical Pathology (ASCP) and the American Society for Clinical Oncology (ASCP), among others [11–12]. The cost effectiveness of such a screening approach has been proven by several studies [13].
Diagnosis
Diagnosis of dMMR tumours is either via PCR amplification of specific microsatellite repeats in formalin-fixed, paraffin-embedded tumour tissue or by immunohistochemistry (IHC) which confirms the absence or presence of MMR proteins. Both MSI testing and IHC have virtually equivalent informative value in predicting germline mutation [3, 14]. Given that IHC is more widely available in general pathology laboratories and is a rapid, efficient and cost-effective method of testing, it is the more frequently used test. It also has the added benefit of directing germline testing to the particular mutated gene.
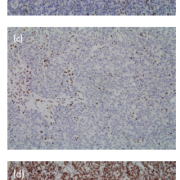
A number of commercially available MMR IHC antibodies are available for laboratory use. A protocol using a panel of four immunohistochemical antibodies to the four mismatch repair gene proteins (MLH1, MSH2, MSH6, PMS2) is recommended (Fig. 1). Complete loss of expression of one or more MMR protein is suggestive of dMMR. Loss of MLH1 often occurs in conjunction with loss of PMS2. This is due to the fact that MLH1 protein forms a heterodimer complex with PMS2. Isolated loss of PMS2 Is indicative of a defect in the PMS2 gene. However, combined loss of PMS2 and MLH1 indicates the defect lies in MLH1, as MLH1 confers stability to PMS2. A similar situation is seen with MSH2 and MSH6; isolated loss of MSH6 indicating defective MSH6, whereas loss of expression of both proteins indicates the defect involves MSH2. Background positive IHC staining in intratumoural lymphocytes or of adjacent normal colonic epithelium, if present, serve as reliable internal positive controls [5].
Once loss of expression of any IHC MMRP is confirmed, further testing is required. In cases where there is loss of MLH1, testing for the presence of BRAF V600E mutation and MLH1 hypermethylation, as mentioned previously, can further stratify those patients who likely have sporadic dMMR tumours. Patients demonstrating loss of MSH2, MSH6 or PMS2, and patients demonstrating loss of MLH1 who are BRAF V600E negative and MLH hypermethylation negative, should undergo germline testing to confirm Lynch syndrome (Fig. 2).
MMR IHC testing is typically performed on CRC resection specimens. Data has recently begun to accumulate that the yield of IHC testing performed on endoscopic biopsy material may be as good as that performed on surgical resections. We recently published a study evaluating the reliability of MMR IHC in CRC from preoperative endoscopic biopsy tissue when compared to matched surgical resection specimens and demonstrated 100% concordance in 53 cases of dMMR (n=10) and pMMR (n=43) tumours [14]. Our results corroborate the results of other studies that indicate endoscopic biopsies are a suitable source of tissue for MMR IHC analysis [15–17].
Preferential testing of MMR status on endoscopic biopsy samples over resection specimens carries a number of advantages. Immunostaining is highly sensitive to the degree of tissue fixation; given the small size of biopsy samples, faster and more thorough fixation may result in superior quality staining. Additionally, neoadjuvant chemoradiotherapy used in the standard treatment of locally advanced rectal tumours may result in a complete pathologic response, with no residual tumour available for testing. Neoadjuvant treatment can also occasionally alter the MMRP status of the tumour. In these two scenarios, the pretreatment biopsy could provide reliable testing material.
Endoscopic biopsies could also be used to initiate earlier and indeed preoperative genetic testing, allowing informed clinical decisions regarding the extent of resection to be made before surgery in those patients confirmed as having Lynch syndrome. The option of total colectomy as an alternative to segmental colectomy could be discussed, particularly with younger patients, to reduce the risk of metachronous CRC and the need for intense postoperative surveillance. In addition, females identified as having Lynch syndrome, who have completed their families, could be considered for concurrent hysterectomy, with/without bilateral salpingo-oophorectomy, in order to prevent the development of a gynecological tract malignancy and spare them a potential additional future procedure.
Recent studies suggest that dMMR tumours may respond well to immunotherapy in patients with advanced disease [9]. In the instance that an advanced tumour is inoperable at diagnosis, metastatic or endoscopic biopsy tissue could be used to screen for dMMR and Lynch syndrome, and direct immunotherapy.
Despite these advantages, some limitations exist in the use of IHC to determine MMR status which are not just specific to biopsy tissue. Rare missense mutations have been reported in MLH1 and MSH6 genes that affect MMR protein function but not translation and antigenicity – in this scenario the tumour harbours a defective protein, but one which demonstrates retention of IHC staining, giving a false result [19].
Intratumoural heterogeneity, where there is heterogeneity of MMR protein expression within a single tumour, also represents a potential pitfall [20]. This may be of particular concern in biopsy samples as they represent only a small proportion of a tumour and could erroneously misclassify the MMR status by virtue of inadequate sampling. Another issue is the small size of endoscopic biopsies; adequate material may not be available for IHC. Encouraging generous tumour sampling at the time of biopsy could reduce the risk of such limitations. Heterogeneity in the MMR status of CRC is rare and is thought in many instances to be a result of suboptimal tissue fixation. Given biopsies are usually of small size, adequate fixation of tissue can be assured.
Conclusion
Up to 15–20% of CRCs are of MSI phenotype, secondary to either sporadic methylation-induced silencing or inherited mutations in MMR-related genes. IHC is an effective and reliable testing modality for determining MMR status in CRC. Colorectal endoscopic biopsy and resection specimens are both suitable sources of testing material, with resection specimens currently the preferred specimen type. Endoscopic biopsy samples may become increasingly important as a testing material as the potential of tailored approaches to surgery, chemotherapy and immunotherapy becomes a standard of care in this era of personalized medicine.
References
1. Guinney J, Dienstmann R, Wang X, de Reyniès A, Schlicker A, Soneson C, Marisa L, Roepman P, Nyamundanda G, et al. The consensus molecular subtypes of colorectal cancer. Nat Med 2015; 21(11): 1350–1356.
2. Poulogiannis G, Frayling IM, Arends MJ. 2010. DNA mismatch repair deficiency in sporadic colorectal cancer and Lynch syndrome. Histopathology 2010; 56(2): 167–179.
3. Lindor NM, Burgart LJ, Leontovich O, Goldberg RM, Cunningham JM, Sargent DJ, Walsh-Vockley C, Petersen GM, Walsh MD, et al. Immunohistochemistry versus microsatellite instability testing in phenotyping colorectal tumors. J Clin Oncol 2002; 20(4): 1043–1048.
4. Bouzourene H, Hutter P, Losi L, Martin P, Benhattar J. Selection of patients with germline MLH1 methylation and BRAF mutation. Fam Cancer 2010; 9: 167–172.
5. Richman S. Deficient mismatch repair: read all about it (Review). Int J Oncol 2015; 47: 1189–1202.
6. Saridaki Z, Souglakos J, Georgoulias V. Prognostic and predictive significance of MSI in stages II/III colon cancer. World J. Gastroenterol 2014; 20(22): 6809–6814.
7. Guastadisegni C, Colafranceschi M, Ottini L, Dogliotti E. Microsatellite instability as a marker of prognosis and response to therapy: a meta-analysis of colorectal cancer survival data. Eur J Cancer 2010; 46(15): 2788–2798.
8. Mohan HM, Ryan E, Balasubramanian I, Kennelly R, Geraghty R, Sclafani F, Fennelly D, McDermott R, Ryan EJ, et al. Microsatellite instability is associated with reduced disease specific survival in stage III colon cancer. Eur J Surg Oncol 2016; 42(11); 1680–1686.
9. Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Eng J Med 2015; 372(26): 2509–2520.
10. Mukherjee A, McGarrity TJ, Ruggiero F, Koltun W, McKenna K, Poritz L, Baker MJ. The revised Bethesda guidelines: extent of utilization in a university hospital medical center with a cancer genetics program. Hered Cancer Clin Pract 2010; 8: 9.
11. Diagnostics guidance 27 (DG27). Molecular testing strategies for Lynch syndrome in people with colorectal cancer. NICE 2017 (https: //www.nice.org.uk/guidance/dg27).
12. Sepulveda AR, Hamilton SR, Allegra CJ, Grody W, Cushman-Vokoun AM, Funkhouser WK, Kopetz SE, Lieu C, Lindor NM, et al. ASCO, A. C. A. Molecular Biomarkers for the Evaluation of Colorectal Cancer: Guideline From the American Society for Clinical Pathology, College of American Pathologists, Association for Molecular Pathology, and the American Society of Clinical Oncology. J Clin Oncol 2017; 35: 1453–1486.
13. Snowsill T, Huxley N, Hoyle M, Jones-Hughes T, Coelho H, Cooper C, Frayling I, Hyde C. A systematic review and economic evaluation of diagnostic strategies for Lynch syndrome. Health Technol Assess 2014; 18(56): 1–406.
14. Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, Clendenning M, Sotamaa K, Prior T, et al. Feasibility of screening for Lynch syndrome among patients with colorectal cancer. J Clin Oncol 2008; 26: 5783–5788.
15. O’Brien O, Ryan É, Creavin B, Kelly ME, Mohan HM, Geraghty R, Winter DC, Sheahan K. Correlation of immunohistochemical mismatch repair protein status between colorectal carcinoma endoscopic biopsy and resection specimens. J Clin Pathol 2018; 71(7): 631–636.
16. Kumarasinghe AP, de Boer B, Bateman AC, Kumarasinghe MP. DNA mismatch repair enzyme immunohistochemistry in colorectal cancer: a comparison of biopsy and resection material. Pathology 2010; 42(5): 414–420.
17. Warrier SK, Trainer AH, Lynch AC, Mitchell C, Hiscock R, Sawyer S, Boussioutas A, Heriot AG. Preoperative diagnosis of Lynch syndrome with DNA mismatch repair immunohistochemistry on a diagnostic biopsy. Dis Colon Rectum 2011; 54(12): 1480–1487.
18. Vilkin A, Leibovici-Weissman Y, Halpern M, Morgenstern S, Brazovski E, Gingold-Belfer R, Wasserberg N, Brenner B, Niv Y, et al. Immunohistochemistry staining for mismatch repair proteins: the endoscopic biopsy material provides useful and coherent results. Hum Pathol 2015; 46(11): 1705–1711.
19. Klarskov L, Holck S, Bernstein I, Okkels H, Rambech E, Baldetorp B, Nilbert M. Challenges in the identification of MSH6-associated colorectal cancer: rectal location, less typical histology, and a subset with retained mismatch repair function. Am J Surg Pathol 2011; 35(9): 1391–1399.
20. Watson N, Grieu F, Morris M, Harvey J, Stewart C, Schofield L, Goldblatt J, Iacopetta B. Heterogeneous staining for mismatch repair proteins during population-based prescreening for hereditary nonpolyposis colorectal cancer. J Mol Diagn 2007; 9: 472–478.
The authors
Dr Odharnaith O’Brien* MB BCh BAO, Dr Éanna Ryan MB BCh BAO, and Prof. Kieran Sheahan MB BCh BAO
Department of Pathology, St. Vincent’s
University Hospital, Dublin, Ireland
*Corresponding author
E-mail: odharnaithobrien@ gmail.com